20 Jun Plantar Fasciitis Explained – Part I
Plantar fasciitis is a condition that causes heel pain and affects thousands of people.
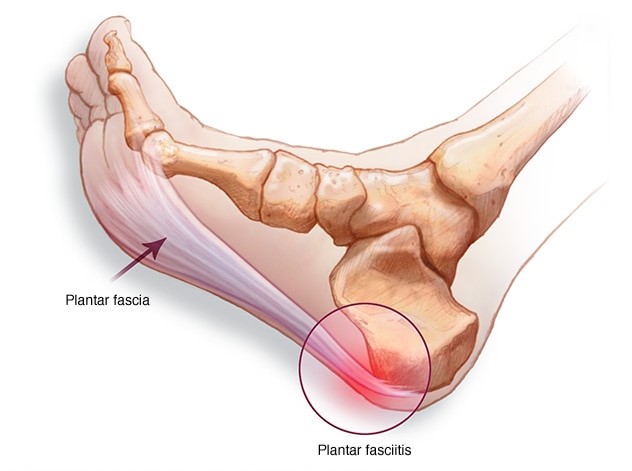
Supporting the arch, the plantar fascia, a thick band of tissue connecting the heel to the ball of the foot, can become inflamed or can tear. You experience pain when you put weight on your foot—particularly when taking your first steps in the morning. The pain can be felt at the heel, or along the arch and the ball of the foot, and the condition develops when repeated weight-bearing activities put a strain on the plantar fascia.
Plantar Fasciopathy is a degenerative Process characterized by Collagen Breakdown, nerve and vascular ingrowth. In late stages of the condition it can progress to Calcification. The correct term for this condition should be Fasciopathy since there is no real inflammatory process involved. As with Achilles Tendinopathy, there are structural changes in the Fascia as a result of collagen breakdown that cause pain rather that inflammation.
Incidence and Causes of Plantar Fasciitis in Runners
Incidence
Plantar fasciitis occurs most frequently in people in their 40s but can occur in all age groups. The condition can develop in athletes who run a great deal and in non-athletes who are on their feet most of the day, such as police officers, cashiers, or restaurant workers, and it occurs in as many as 2 million Americans per year and 10% of the population over their lifetimes.
Plantar fasciitis affects people of all ages, both athletes and non-athletes. Men and women have an equal chance of developing the condition.
Causes of Plantar fasciitis
Factors that contribute to the development of plantar fasciitis include:
- Age (over 40 years)
- A job, sport, or hobby that involves prolonged standing or other weight-bearing activity
- Rapid increases in length or levels of activity, such as beginning a new running program or changing to a job that requires a lot more standing or walking than you are accustomed to
- Decreased calf muscle flexibility
- Increased body weight (Body Mass Index greater than 30)
- Tendency to have a flat foot (pronation)
When we consider the Running Population only, Plantar Fasciitis may be linked to:
- Quick or sharp changes in training : increased pace, change of footwear or foot strike
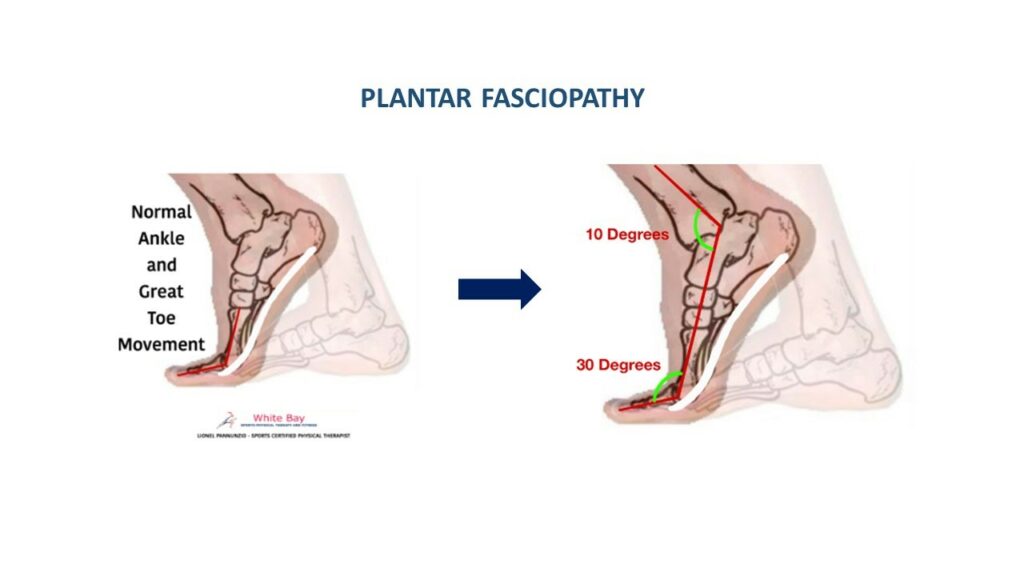
- Reduced ankle dorsiflexion in combination with reduced Great Toe Extension.
- Reduced Toe flexor and evertor strength and decreased Hamstring Flexibility ( Sullivan et al 2015)
- Decreased Calf capacity
Plantar fasciitis highly related to tightness in Calf muscles?
In the picture below you can appreciate how the ankle and the great toe work together to push the body forward when walking or running . You can also see how a normal combined movement between Ankle Dorsiflexion and Great toe Extension are necessary to avoid excessive tension in the fascia. Any restrictions in these joints or their surrounding muscles will create excessive loading in the fascia creating the Fasciopathy if the movement is not restored.
Signs and Symptoms
People with plantar fasciitis may experience pain:
- In the morning, when stepping out of bed and taking the first steps of the day
- With prolonged standing
- When standing up after sitting for awhile
- After an intense weight-bearing activity such as running
- When climbing stairs
- When walking barefoot or in shoes with poor support
As your body warms up, your pain may actually decrease during the day but then worsen again toward the end of the day because of extended walking. Severe symptoms may cause you to limp.
How is it diagnosed?
The physical therapist’s diagnosis is based on your health and activity history and a clinical evaluation. Your therapist also will take a medical history to make sure that you do not have other possible conditions that may be causing the pain. Sharing information about the relationship of your symptoms to your work and recreation, and reporting any lifestyle changes, will help the physical therapist diagnose your condition and tailor a treatment program for your specific needs.
To diagnose plantar fasciitis, your therapist may conduct the following physical tests to see if symptoms occur:
- Massaging and pressing on the heel area (palpation)
- Gently stretching the ankle to bend the top of the foot toward the leg (dorsiflexion)
- Gently pressing the toes toward the ankle
How Physical Therapy can help?
First of all, Plantar fasciopathy should ruled-in and other conditions like fat pad irritation, stress fractures, nerve entrapment or arthropathies should be ruled-out .
Once you are diagnosed with plantar fasciitis, your physical therapist will work with you to develop a program to decrease your symptoms that may include:
- Improve the flexibility of your ankle and the plantar fascia
- Use of a night splint to maintain correct ankle and toe positions
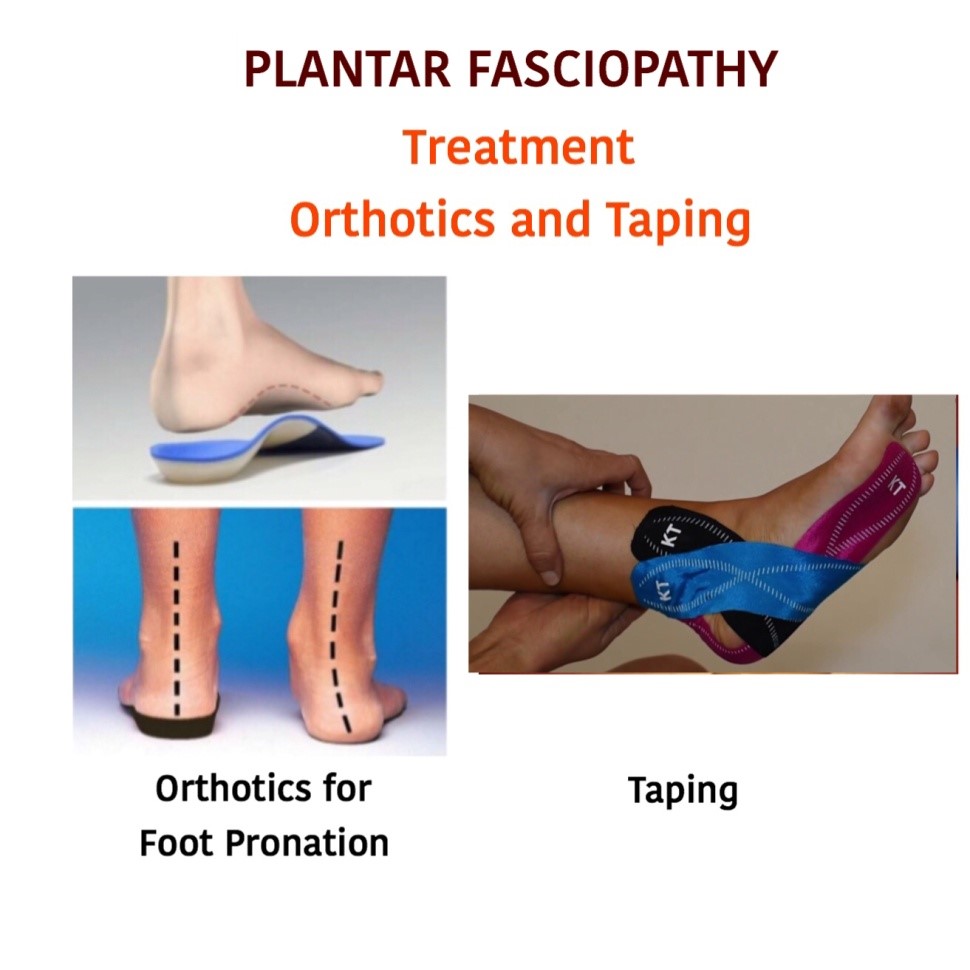
- Selection of supportive footwear and/or shoe inserts that minimize foot pronation and reduce stress to the plantar fascia
- Iontophoresis (a gentle way to deliver medication through the skin)
- Taping of the foot to provide short-term relief
- Increase Plantar Flexor capacity
- Increase Great Toe mobility and Range of movement
- Increase strength and flexibility of the Lower Extremity as a whole.
Research shows that most cases of plantar fasciitis improve over time with these conservative treatments, and surgery is rarely required.
Plantar Fasciopathy is a self-limiting condition of variable duration
With treatment symptoms usually improved in 3-6 months (some cases up to 9 months)
Stages of Rehabilitation
Pain Dominant Phase
Plantar Fascia becomes sensitive to load. Pain and stiffness occur when stepping out of bed and taking the first steps of the day, and also pain with activities like walking long distance or prolonged standing. This phase can last 2-8 weeks.
Interventions
- Control pain by reducing or modifying aggravating Activities: load management , reduce running distance or frequency
- Improve the flexibility of your ankle and the plantar fascia: mobility work for ankle and foot with emphasis on reducing tightness in calf and posterior chain.
- Increase Plantar Flexor capacity: mainly Isometric strengthening progressing to light Isotonic strengthening as tolerated
- Increase Great Toe mobility and Range of movement: big emphasis on Improving Great toe extension to help with shock absorption and power generation in the stride
- Increase strength and flexibility of the Lower Extremity as a whole: quadriceps and Gluteal muscles assist with load absorption during the run so by strengthening these muscles group we help unloading the fascia.
Plantar Fascia Mobilization – Stretch
In sitting with the foot resting on your opposite knee, bend the ankle and big toe up holding for 10 -15 seconds and repeat 10 times
Ankle Strengthening
Turn the ankle out against the band and then in . 8-12 reps to each side
Isometric Toe Flexion
Push the big toe down as hard as possible and tolerated, Hold the contraction for 3 seconds . Repeat 5-10 times each foot.
Also in the Pain Dominant Phase we must address any excessive foot deviation by using over-the-counter orthotics or Taping for short-term pain management. If these help it may grant the investment in custom-made orthotics down the road.
Load Dominant Stage
Pain at first step in the morning improves and increases walking tolerance. Symptoms remain stable unless the fascia is overloaded.
Interventions:
- Increase Plantar Flexor capacity: progressing from Isotonics to Eccentric movements of the calf
- Interval training to increase load capacity to develop calf endurance and Power : plyometrics.
- Establish a Return to Run Strategy: identify distance or pace that patient can run without pain and build up from there a distance or pace progression to minimize irritation of the fascia and allow proper loading on these tissues
- Gait and run retraining: Increase step rate to minimize longer ground contact times, large vertical oscillations. Minimize rear foot eversion .
The following exercises are intended to create ankle Dorsiflexion and Great toe extension and at the same time mobility and strengthening of the plantar fascia and calf-ankle-foot- Toe complex muscles.
Great Toe sliders
Great Toes – Plantar Fascia Strengthening – Push off
Conclusion
- Plantar Fasciopathy and heel pain affect a large population of runners
- Conventional physical or chiropractic treatment usually fails to address all the possible causes of this condition
- Improve and restore plantar fascia length and Plantar Flexion Capacity with emphasis on Great Toe strength are the main goals of the treatment.
- Our comprehensive approach is backed-up by the most recent research. Once you resolve the root of the problem the Plantar Fascia becomes pain free
- Education and load management are key factors for people with Plantar Fasciopathy
Do you have any questions? Drop a note, we’d love to hear from you.
Sign Up and ask the Therapist.
Lionel Pannunzio is a Physical Therapist and Board-Certified Sports Specialist, owner of White Bay Physical Therapy.
He has been helping runners for more than 20 years
“Keeping Athletes in the game”
With offices located at 17180 Royal Palm Blvd – Weston – Florida – 33326
You can reach him at 754-244-2561
Visit his website: www.wbsphysicaltherapy.com
[email protected]

Sorry, the comment form is closed at this time.