
27 May Achilles Pain (Tendinopathy) Explained – Part I
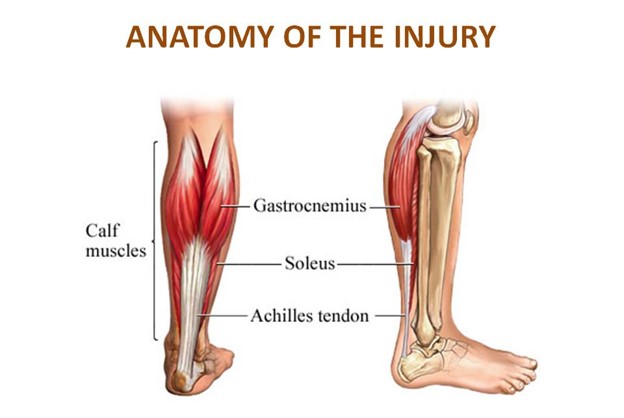
Achilles tendinopathy (also tendonitis or tendinosis) is an irritation of the Achilles tendon, a thick band of tissue along the back of the lower leg that connects the calf muscles to the heel that results in pain, swelling, and impaired function.
The term “tendinopathy” refers to any problem with a tendon, either short- or long-term.
The Achilles tendon transmits force from the calf muscles down to the foot when a person pushes the foot off the ground (eg, runs or jumps), and helps control the position of the ankle when the foot touches back down on the ground (eg, lands).
Achilles tendinopathy results when the demand placed on the Achilles tendon is greater than its ability to function.
The condition can occur after a single incident (acute injury) or after repetitive irritation or “microtrauma” (chronic injury).
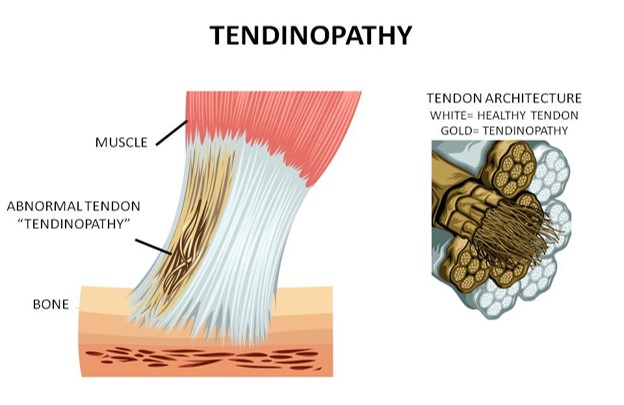
Most often, Achilles tendon pain is the result of repetitive trauma to the tendon that can result in chronic Achilles tendinopathy—a gradual breakdown of the tissue—and is most often treated with physical therapy. Please note that we don’t use the term tendonitis because “itis” means inflammation like in a acute ankle sprain. This is more a problem in the architecture of the tendon, a mechanical problem within the tendon and not an inflammatory process.
So in the tendinopathy there are mainly healthy fibers in conjunction with some “abnormal fibers”.
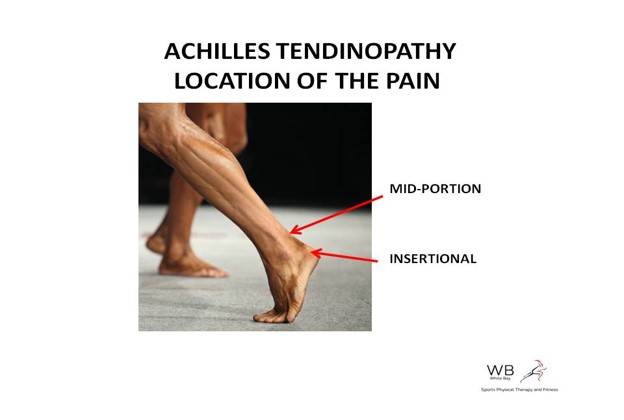
Pain can be present at any point along the tendon; the most common area to feel tenderness is just above the heel (known as midportion Achilles tendinopathy), although it may also be present where the tendon meets the heel (known as insertional Achilles tendinopathy).
Causes
Achilles tendinopathy is linked to several different factors, including:
- Calf muscle tightness
- Calf muscle weakness
- Abnormal foot structure
- Abnormal foot mechanics
- Improper footwear
- A change in an exercise routine or sport activity
- Obesity
Symptoms
With Achilles tendinopathy, you may experience:
- Tenderness in the heel or higher up in the Achilles tendon with manually applied pressure
- Pain and stiffness with walking, at its worst with the first several steps, escially worse in the morning upon stepping down from bed or after being sitting for +20-30 mins
- Tightness in the calf
- Swelling in the back of the ankle
The Pain cycle and the road to a Chronic pain
In the beginning of the tendinopathy the pain will be present at the begining of the run but it will disappears quick once warm-up. Then pain will not disappear after warm-up and will be present throughout the run. Finally the pain will severe and you can’t run comfortably anymore
That’s how this Tendinopathy becomes Chronic and from there it can last forever without proper treatment
Do I need Xrays or expensive MRIs ?
Your doctor (what we do at White Bay Physical Therapy) will review your medical history and complete a thorough examination of your heel, ankle, and calf. Your foot posture, strength, flexibility, and movement will be assessed. This process may include watching you stand in a relaxed stance, walk, squat, step onto a stair, or do a heel raise. The motion and strength in other parts of your leg also will be assessed.
You may also be asked questions regarding your daily activities, exercise regimens, and footwear, to identify other contributing factors to your condition.
Imaging techniques, such as X-ray or MRI, are often not needed to diagnose Achilles tendinopathy. Although it is unlikely that your condition will ultimately require surgery, your physical therapist will consult with other medical professionals, such as an orthopedist, to determine the best plan of treatment for your specific condition if it does not respond to conservative care.
Treatment Guidelines
Seth O’Neil a physiotherapist from UK and one the Achilles Tendinopathy “Gurus” resumed the guidelines for treating Achilles Tendinopathy in 5 points
- Reassurance: one of the common incorrect beliefs is that tendinopathy needs to be rested to get better. In actuality the tendon needs to be used ‘more’ but in the correct manner (ie loaded rehab exercises and running
- De-threaten the condition: many people can fear loading the tendon for concern of ‘tears’ or ‘rupture’. The astute therapist’s job is to educate the tendon pain sufferer of the high loads that tendons endure day to day (eg 4x Body-weight intra tendon loads with walking, 6x BW with running) so loading the tendon with just your body at the beginning it is not a high demand activity so you are safe to do it
- Educate on load management: the runner needs to appreciate that loading tendon correctly is the pathway forward, how to monitor increases in workload based on the pain response, the required time to allow tendon to adapt to loading, why ‘flare ups’ can be expected.
- Build plantar flexor capacity: as I so often say ‘below the knee if the key’. I like to see runners being able to do heavy gastrocnemius and soleus work in a gym (targets 1.5x body weight soleus seated calf raises & 0.3-0.4x body weight standing calf raises aiming for 3x 8reps with good control
- Return to full running: this must be staged & I normally suggest building volume, before adding speed, and latter hills
In Part II we will talk about the exercises you can do to self manage Achilles Pain.
===>> Continue to Part II
Do you have any questions? Drop a note, we’d love to hear from you.
Sign Up and ask the Therapist.

Sorry, the comment form is closed at this time.